Patriarchy, which is an academic term simply explaining the dominance of men in our society, is one of the most pervasive social phenomena. The crucial aspect of understanding patriarchy is realising how it influences every aspect of the world, but perhaps even more significantly, how it shapes our opinion and perception of the world itself. Our subconscious biases and beliefs are rooted in the patriarchal conditioning we receive growing up, and accordingly, any attempt at being gender-sensitive must begin with a critical self-questioning of these hidden biases.
Patriarchal biases are likely to reveal themselves in places you’d least suspect. One such unassuming place is the field of medicine.
From the ancient Greeks deeming menstruation a result of ‘too much’ blood accumulation in women’s bodies to all and any health conditions suffered by women being blamed on ‘hysteria,’ the medical field hardly has a gender-inclusive history. Even though our knowledge of female anatomy and occurrences such as menstruation, pregnancy, and hormonal cycles has come far since then, the healthcare system continues to operate on a ‘male default’ basis, as evidenced by diagnostic trends, clinical trials for new drugs and treatments, and the gap in research, which will be discussed shortly.
It is in this context that the phenomenon of women’s pain being systematically dismissed or diminished by medical professionals has been termed as the ‘gender pain gap.’ Coined by Diane Hoffmann and Anita Tarzian in their 2008 paper titled ‘The Girl Who Cried Pain: A Bias Against Women in the Treatment of Pain,’ this phrase refers to the manner in which ingrained gender stereotypes lead to women’s pain being far less treated, ignored, and more likely to be blamed on psychological or emotional causes than bodily ones. This is despite the fact that numerous studies indicate that women suffer from chronic pain more so than men do and that there exist reproductive health issues such as endometriosis, PCOD, and PCOS, among others, that can cause severe debilitating pain in its patients.
The causes that feed into this gap are many. Inarguably, the most fundamental is the aforementioned patriarchal bias that has shaped the course of research and development in the medical field. As Caroline Perez investigated in her 2019 book ‘Invisible Women: Exposing Data Bias in a World Designed for Men,’ our modern scientific understanding of the world is built on data sets that are either entirely exclusive or inadequately representative of women. Most commonly prescribed drugs today, including over-the-counter painkillers, were initially never tested on women, let alone taken into account for their efficacy and side effects on people at different stages of their menstrual cycle. Moreover, the dominant cultural narrative that normalises pain, from period cramps to pregnancy, as a ‘natural’ part of womanhood has only added to the problem as women continue to self-dismiss or not seek professional help for the pain they experience.
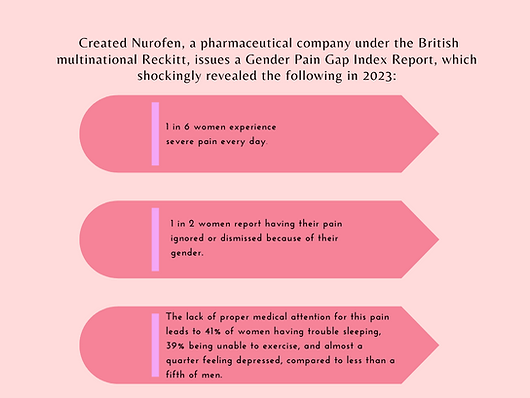
The fact of the matter is that the gender pain gap has serious repercussions and constitutes a serious health problem affecting millions worldwide today. Nurofen, a pharmaceutical company under the British multinational Reckitt, issued a Gender Pain Gap Index Report in 2023, which shockingly revealed the following:
- 1 in 6 women experiences severe pain every day.
- 1 in 2 women report having their pain ignored or dismissed because of their gender.
- The lack of proper medical attention for this pain leads to 41% of women having trouble sleeping, 39% being unable to exercise, and almost a quarter feeling depressed, compared to less than a fifth of men.
Furthermore, studies find that women are more likely to be offered minor tranquillizers and antidepressants than analgesic pain medication, along with being referred for further diagnosis at a lower rate. There exists a plethora of anecdotal evidence to substantiate this as social media is brimming with women recounting personal stories of severe period cramps being dismissed only to find out later that they were suffering from issues like endometriosis, being offered minimal pain-relief medications during the insertion procedure for intrauterine devices, and historical tales of the origin of the “husband-stitch” and why women lie down while giving birth. All of this paints a clear picture of the kind of systemic neglect women continue to suffer at the hands of the medical field even today.
All of this is not to say that all doctors and medical professionals are consciously denying women their right to good health but to recognise that there exist certain patriarchal biases that are so deeply ingrained in our collective psyche, that they have gone altogether unchecked over the years. Indeed, we must interrogate and become conscious of the same in order to make healthcare more accessible and inclusive for all genders. There is a need for more significant funding to promote research on these issues, as well as the gender sensitisation of medical professionals to become cognizant of the pain gap inherent in their practices.